Engineers from the Massachusetts Institute of Technology (MIT), in partnership with scientists at the Cancer Research UK Manchester Institute, have created a novel method of growing small copies of the pancreas, which can be made from either healthy or malignant cells. Scientists hope that their new models may aid them in the development and testing of possible treatments for pancreatic cancer, which is presently one of the most difficult kinds of cancer to cure.
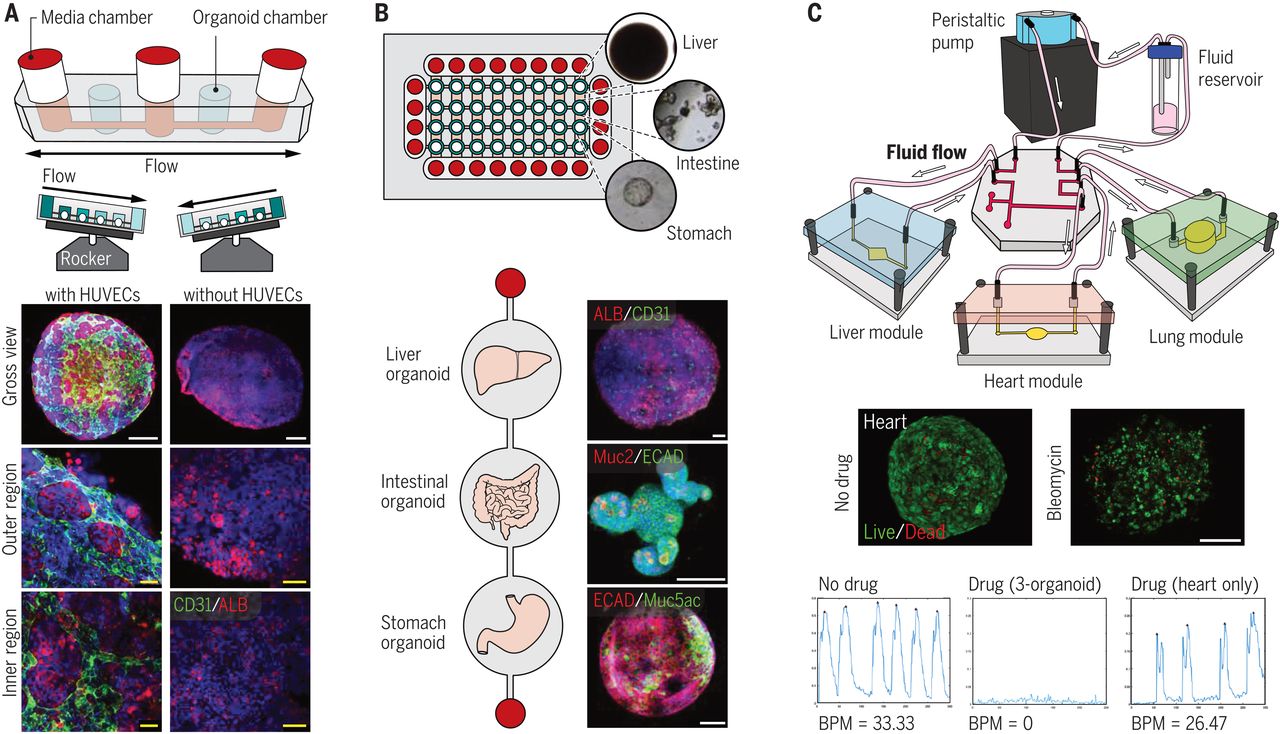
The researchers were able to develop pancreatic “organoids” in a customised gel that mimicked the extracellular environment surrounding the pancreas, enabling them to explore the crucial interactions between pancreatic cancers and their surrounding environment. To distinguish it from some of the gels already in use for tissue growth, the new MIT gel is totally synthetic, simple to build, and can be made with a consistent composition every time.
According to Linda Griffith, the School of Engineering Professor of Teaching Innovation and a professor in both biological engineering and mechanical engineering, “reproducibility is a significant concern.” In order to undertake more systematic cultures of these sorts of organoids, and in particular to regulate the microenvironment, the scientific community has been exploring for methods to do so.”
Researchers have also shown that their novel gel may be used to produce different forms of tissue, including intestinal and endometrial tissue, according to their findings.
Among the senior authors of the work, which appears today in Nature Materials, are Griffith and Claus Jorgensen, a group leader at the Cancer Research UK Manchester Institute in Manchester, England. Among the authors is Christopher Below, a former graduate student at the Cancer Research UK Manchester Institute who is now working as a freelance writer.
Creating a microenvironment that is similar to the real one
Organoids grown in a lab dish have traditionally been grown using commercially available tissue-derived gel, which may be purchased online. In spite of this, Griffith notes that since the most extensively used commercial gel is a complicated combination of proteins, proteoglycans, and growth factors produced from a tumour established in mice, it is varied from lot to lot and may include unwanted components. It also does not always allow for the proliferation of a variety of cell types to coexist. It was around ten years ago that Griffith’s lab began working on developing a synthetic gel that could be used to grow epithelial cells, which form the sheets that coat the inside of most organs, as well as other supporting cells in culture.
The gel that they created is based on polyethylene glycol (PEG), a polymer that is often utilised in medical applications since it does not interact with live cells in the same way that other materials do. In order to better understand the biochemical and biophysical properties of the extracellular matrix, which is the layer of tissue that surrounds organs in the body, the researchers studied the extracellular matrix and identified characteristics that could be incorporated into the PEG gel to aid in the growth of cells in it.
One distinguishing characteristic is the presence of small molecules known as peptide ligands, which bind with cell surface proteins known as integrins. Cells cling to the gel and form organoids as a result of the sticky binding that occurs between ligands and integrins. Small synthetic peptides generated from fibronectin and collagen were added to the gels, and the researchers discovered that this enabled them to produce a range of epithelial tissues, including intestinal tissue. Additionally, they demonstrated that supporting cells known as stromal cells, in addition to immune cells, may flourish in this environment.
Griffith and Jorgensen sought to investigate whether the gel could be utilised to promote the development of normal pancreatic organoids as well as pancreatic cancers in the latest investigation. Since a result, it has traditionally been difficult to develop pancreatic tissue in a way that mimics both the malignant cells and the surrounding environment, as pancreatic tumour cells lose their dangerous characteristics after they have been removed from the body.
A process for producing the novel gel was created by Griffith’s group, which then collaborated with Jorgensen’s lab, which investigates the biology of pancreatic cancer, to put it through its paces. Jorgensen and his students were able to create the gel and utilise it to develop pancreatic organoids from either healthy or malignant pancreatic cells taken from mice, according to the researchers.
It was a simple process after we received the protocol from Linda and placed the chemicals in the system, according to Jorgensen. “I believe it says volumes about how resilient the system is, as well as how simple it is to put it into practise in the lab.”
He claims that other procedures they had explored were either too complex or did not accurately replicate the microenvironment seen in real tissues. When Jorgensen’s group used this gel to compare the pancreatic organoids to tissues that they had previously analysed in real mice, the researchers discovered that the tumour organoids expressed a number of the same integrins as were identified in pancreatic tumours. Other kinds of cells that often surround tumours, such as macrophages (which are immune cells) and fibroblasts (which are supporting cells), were also able to thrive in the tumour microenvironment.
Cells obtained from patients
Aside from this, the researchers demonstrated that they could utilise their gel to create organoids from pancreatic cancer cells obtained from patients. They think it might also be valuable in the research of malignancies such as lung, colorectal, and other types. Such systems might be used to investigate the effects of putative cancer medicines on tumours and their surrounding microenvironment.
Furthermore, Griffith intends to utilise the gel to grow and examine tissue obtained from people suffering from endometriosis, a disorder in which the tissue that lines the uterus begins to proliferate outside of the body. This might cause discomfort and, in some cases, infertility.
Its synthetic nature means that it can be readily created in a laboratory by combining specified precursors, such as PEG and certain polypeptides. This is one of the benefits of the new gel. According to the researchers, they have submitted a patent application for their invention and are now in the process of licencing it to a firm that might manufacture the gel on a commercial scale.
In addition to Cancer Research UK and the Rosetrees Trust, the research was supported by a European Research Council Consolidator Award as well as funding from the National Science Foundation. The National Institutes of Health and the Defense Advanced Research Projects Agency provided additional support.
For More Information Visit : Tiimez Magaizne